-
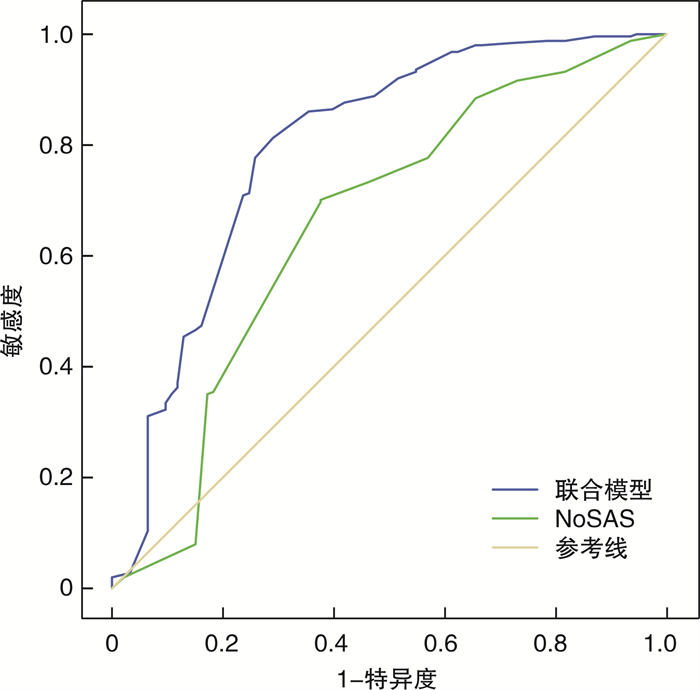
摘要: 目的 评价改良Mallampati分级联合NoSAS问卷筛查阻塞性睡眠呼吸暂停(OSA)的价值。方法 以因睡眠障碍就诊的344例患者为研究对象,测量所有患者的身高、体重、颈围等参数,填写NoSAS量表及评估改良Mallampati分级。对患者均进行PSG记录,根据PSG监测结果中的AHI将患者分为非OSA组(AHI < 5)93例和OSA组251例,OSA组包括轻度OSA组(AHI为5~15)、中度OSA组(AHI为16~30)、重度OSA组(AHI>30)。绘制受试者工作特征(ROC)曲线,分别评估NoSAS评分和NoSAS评分联合改良Mallampati分级对OSA的筛查价值。结果 以NoSAS≥8分为标准筛查OSA组的灵敏度和特异度分别为0.733和0.538;以NOSAS≥9分为标准筛查OSA的灵敏度和特异度分别为0.701和0.624;采用NoSAS联合改良Mallampati分级筛查OSA的灵敏度及特异度分别为0.813和0.710。结论 NoSAS问卷作为一项新的筛查工具,简单便捷。改良Mallampati分级联合NoSAS问卷可明显提高对OSA的筛查敏感性及特异性,有较高的应用价值。
-
关键词:
- 阻塞性睡眠呼吸暂停 /
- NoSAS问卷 /
- 改良Mallampati分级 /
- 多导睡眠监测
Abstract: Objective To evaluate the value of improved Mallampati grading combined with NoSAS questionnaire in screening for obstructive sleep apnea (OSA).Method A total of 344 patients admitted to our hospital for sleep disorders were studied. All patients were measured for their height, weight, neck circumference and other parameters. NoSAS scores, improved Mallampati grading and polysomnography (PSG) were performed in these patients. According to AHI in PSG monitoring results, patients were divided into non-osa group (AHI < 5) 93 cases and OSA group 251 cases. The OSA group were divided into mild (AHI 5-15), moderate(AHI 16-30) and severe OSA group(AHI>30) according to the PSG result. The ROC curve was plotted to evaluate the screening value of NoSAS and improved Mallampati grading combined with NoSAS for OSA.Result With the NoSAS score of 8 or 9 as cutoffs for analysis, the sensitivity for OSA was 0.733 and 0.701; the specificity for OSA was 0.538 and 0.624, respectively. The sensitivity and specificity of NoSAS combined with improved Mallampati grading for screening OSA were 0.813 and 0.710, respectively.Conclusion As a new screening tool, NoSAS questionnaire is simple and convenient, and has certain screening value to OSA. The improved Mallampati grading combined with NoSAS questionnaire can obviously improve the screening sensitivity and specificity of Osa, and has higher application value. -

-
表 1 患者的基本资料
项目 OSA组 非OSA组 P 男/女 213/38 71/22 0.064 年龄/岁 45.98±12.80 51.42±16.14 0.004 BMI 29.03±5.92 25.48±3.20 < 0.001 颈围/cm 41.00(39.00,43.00) 39.00(36.00,41.00) < 0.001 改良Mallampati分级 < 0.001 Ⅰ级 5(2.0) 31(33.3) Ⅱ级 40(15.9) 34(36.6) Ⅲ级 122(48.6) 19(20.4) Ⅳ级 84(33.5) 9(9.7) NoSAS评分 11.00(8.00,13.00) 8.00(5.00,11.00) < 0.001 表 2 NoSAS联合改良Mallampati分级对于筛查OSA的Logistics回归模型
回归系数 标准误 Wald P AHI ≥5 NoSAS评分 -0.03 0.05 0.44 0.508 改良Mallampati分级 1.48 0.20 54.62 < 0.001 截距 -2.61 0.49 28.91 < 0.001 AHI>15 NoSAS评分 -0.02 0.04 0.22 0.639 改良Mallampati分级 1.23 0.18 48.58 < 0.001 截距 -2.90 0.47 37.72 < 0.001 AHI>30 NoSAS评分 0.02 0.04 0.34 0.561 改良Mallampati分级 1.05 0.17 38.27 < 0.001 截距 -3.39 0.50 46.47 < 0.001 表 3 NoSAS评分及联合改良Mallampati分级对OSA的筛查价值
AUC(95%CI) 灵敏度/% 特异度/% 截断值 P AHI ≥5 NoSAS评分 0.656(0.586~0.727) 0.733 0.538 8 < 0.001 联合模型 0.796(0.736~0.856) 0.813 0.710 0.796 <0.001 AHI>15 NoSAS评分 0.630(0.568~0.691) 0.718 0.542 10 < 0.001 联合模型 0.754(0.699~0.809) 0.762 0.676 0.639 < 0.001 AHI>30 NoSAS评分 0.647(0.589~0.705) 0.742 0.508 10 < 0.001 联合模型 0.736(0.684~0.787) 0.871 0.482 0.379 < 0.001 -
[1] 中国医师协会睡眠医学专业委员会. 成人阻塞性睡眠呼吸暂停多学科诊疗指南[J]. 中华医学杂志, 2018, 98(24): 1902-1914. doi: 10.3760/cma.j.issn.0376-2491.2018.24.003
[2] Peppard PE, Young T, Barnet JH, et al. Increased prevalence of sleep-disordered breathing in adults[J]. Am J Epidemiol, 2013, 177(2): 1006-1014.
[3] Sutherland K, Cistulli PA. Recent advances in obstructive sleep apnea pathophysiology and treatment[J]. Sleep Biological Rhythms, 2015, 13(1): 26-40.
[4] 马薇, 王金凤, 谢宇平, 等. 阻塞性睡眠呼吸暂停综合征伴高血压患者睡眠呼吸指数与同步血压特征[J]. 临床耳鼻咽喉头颈外科杂志, 2015, 29(6): 520-524. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201506011.htm
[5] Xie C, Zhu R, Tian Y, et al. Association of obstructive sleep apnoea with the risk of vascular outcomes and all-cause mortality: a meta-analysis[J]. BMI Open, 2017, 7(12): e013983. doi: 10.1136/bmjopen-2016-013983
[6] Marti-Soler H, Hirotsu C, Marques-Vidal P, et al. The NoSAS score for screening of sleep-disordered breathing: a derivation and validation study[J]. Lancet Respir Med, 20l6, 4(9): 742-748. doi: 10.1016/S2213-2600(16)30075-3
[7] Tan A, Hong Y, Tan LWL, et al. Validation of NoSAS score for screening of sleep-disordered breathing in a multiethnic Asian population[J]. Sleep Breath, 2017, 21(4): 1033-1038. doi: 10.1007/s11325-016-1455-4
[8] Samsoon GL, Young JR. Difficult tracheal intubation: a retrospective study[J]. Anaesthesia, 1987, 42(5): 487-490. doi: 10.1111/j.1365-2044.1987.tb04039.x
[9] Hong C, Chen R, Qing S, et al. Validation of the NoSAS score for the screening of sleep-disordered breathing: a hospital-based retrospective study in China[J]. J Clin Sleep Med, 2018, 14(2): 191-197. doi: 10.5664/jcsm.6930
[10] 张笋, 卿思敏, 刘恒, 等. 动脉血HC03-浓度对NoSAS问卷筛查OSA准确性的影响[J]. 中华医学杂志, 2018, 98(32): 2564-2568. doi: 10.3760/cma.j.issn.0376-2491.2018.32.006
[11] 姜宇英, 王翰青, 诸葛盼, 等. 基于不同病情分级的阻塞性睡眠呼吸暂停低通气综合征患者临床因素调查及干预[J]. 中国全科医学, 2017, 20(A3): 25-27. https://www.cnki.com.cn/Article/CJFDTOTAL-QKYX2017S3010.htm
[12] Yagi H, Nakata S, Tsuge H, et al. Morphological examination of upper airway in obstructive sleep apnea[J]. Auris Nasus Larynx, 2009, 36(4): 444-449. doi: 10.1016/j.anl.2008.11.003
[13] Nuckton TJ, Glidden DV, Browner SW, et al. Physical examination: Mallampati Score as an independent predictor of obstructive sleep apnea[J]. Sleep, 2006, 29(7): 903-908. doi: 10.1093/sleep/29.7.903
-

| 引用本文: | 刘坤贺, 张妍蓓. 改良Mallampati分级联合NoSAS问卷筛查OSA的价值[J]. 临床耳鼻咽喉头颈外科杂志, 2020, 34(4): 320-324. doi: 10.13201/j.issn.2096-7993.2020.04.008 |
| Citation: | LIU Kunhe, ZHANG Yanbei. The value of improved Mallampati grading combined with NoSAS in OSA screening[J]. J Clin Otorhinolaryngol Head Neck Surg, 2020, 34(4): 320-324. doi: 10.13201/j.issn.2096-7993.2020.04.008 |
- Figure 1.


 下载:
下载: