Correlation between serum ferritin level and mortality in patients with decompensated liver cirrhosis
-
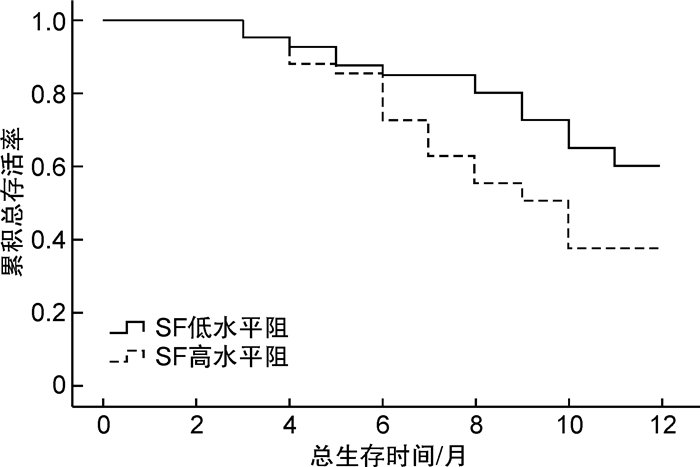
摘要: 目的 探讨血清铁蛋白(SF)水平与肝硬化失代偿患者死亡率的关系。方法 所有患者按照SF水平分为低水平组和高水平组,运用t检验或χ2检验比较2组患者各临床因素,运用Pearson检验对肝硬化失代偿患者血清SF水平与肝肾功和甲胎蛋白进行相关性分析,Kaplan-Meier生存分析比较2组患者随访1年内总生存率,Cox回归分析获得影响肝硬化失代偿患者随访1年内生存情况的独立预测因素。结果 研究共纳入119例肝硬化失代偿患者,其中男80例(67.2%),女39例(32.8%),平均年龄(53.6±13.4)岁,所有患者按照SF水平分为低水平组(< 200 ng/mL)和高水平组(≥200 ng/mL),低水平组57例(47.9%),高水平组62例(52.1%),SF高水平组患者消化道出血、Ⅲ度食管胃底静脉曲张以及腹水所占的比例明显高于SF低水平组患者,SF高水平组患者肌酐、总胆红素、Child-Pugh评分以及MELD评分明显高于SF低水平组患者。Pearson相关性分析显示,肝硬化失代偿患者血清SF与肌酐、总胆红素、Child-Pugh评分以及MELD评分呈明显正相关,Kaplan-Meier生存分析显示,SF低水平组患者随访3个月、6个月、12个月总生存率明显高于SF高水平组患者(93.4%、85.6%、56.7% vs. 93.4%、82.1%、34.6%,P< 0.05)。Cox多因素分析显示,消化道出血、肝性脑病、肌酐、SF、Child-Pugh评分以及MELD评分6个指标为影响肝硬化失代偿患者随访1年内生存情况的独立预测因素,其中SF高水平患者随访1年内死亡的风险是SF低水平患者的1.678倍(HR:1.678,95%CI:1.213~1.994,P=0.037)。结论 SF、Child-Pugh评分和MELD评分可用于预测肝硬化失代偿期患者疾病严重程度和短期预后。
-
关键词:
- 血清铁蛋白水平 /
- 肝硬化失代偿 /
- 死亡率 /
- Child-Pugh评分 /
- MELD评分
Abstract: Objective To investigate the relationship between serum ferritin(SF) level and mortality in decompensated patients with liver cirrhosis.Methods All patients were divided into low-level group and high-level group according to SF level,t-test or χ2test was used to compare the clinical factors of the two groups, use the Pearson test to analyze the correlation between serum SF level, liver and kidney function and alpha fetoprotein in patients with decompensated liver cirrhosis, Kaplan Meier survival analysis was used to compare the overall survival rate of decompensated patients with liver cirrhosis between the two groups within one year of follow-up, and Cox regression analysis to obtain the independent predictors of the survival of patients with decompensated liver cirrhosis within one year of follow-up.Results A total of 119 patients with decompensated liver cirrhosis were included in the study, with an average age of (53.6±13.4) years, including 80 males(67.2%) and 39 females(32.8%). All patients were divided into low-level group(< 200 ng/mL) and high-level group(≥200 ng/mL) according to SF level, 57 cases(47.9%) in low-level group and 62 cases(52.1%) in high-level group. The proportion of gastrointestinal bleeding, grade Ⅲ esophagogastric varices and ascites in the high SF level group was significantly higher than that in the low SF level group. The creatinine, total bilirubin, child Pugh score and MELD score in the high-level SF group were significantly higher than those in the low-level SF group. The Pearson correlation analysis showed that there was a significant positive correlation between serum SF and creatinine, total bilirubin, child Pugh score and MELD score in patients with decompensated liver cirrhosis, Kaplan Meier survival analysis showed that the 3-month, 6-month, 12-month follow-up overall survival rate of patients with decompensated liver cirrhosis in low SF level group was significantly higher than that of patients in high SF level group(93.4%, 85.6%, 56.7% vs. 93.4%, 82.1%, 34.6%,P< 0.05). Cox multivariate analysis showed that gastrointestinal bleeding, hepatic encephalopathy, creatinine, SF Child-Pugh score and MELD score were independent predictors of survival in patients with decompensated liver cirrhosis during 1-year follow-up. The risk of death in patients with high SF level was 1.678 times higher than that in patients with low SF level(HR: 1.678, 95%CI: 1.213—1.994,P=0.037).Conclusion SF, Child-Pugh score and MELD score can be used to predict the disease severity and short-term prognosis of patients with decompensated liver cirrhosis.-
Key words:
- serum ferritin level /
- decompensated liver cirrhosis /
- mortality /
- Child-Pugh score /
- MELD score
-

-
表 1 2组患者一般临床资料比较
临床指标 SF低水平组(n=57) SF高水平组(n=62) t/χ2 P 年龄/岁 53.4±13.8 53.9±13.2 0.912 0.386 男/女 38/19 42/20 1.523 0.126 病因(乙肝/丙肝/其他) 25/10/22 35/12/15 2.017 0.097 食管胃底静脉曲张(Ⅱ度/Ⅲ度) 30/27 21/41 4.396 0.032 消化道出血(是/否) 12/45 30/32 4.125 0.033 腹水(是/否) 28/29 45/17 5.725 0.017 肝性脑病(是/否) 10/47 23/39 2.236 0.095 肌酐/(mmol·L-1) 79.4±25.6 92.3±27.8 8.136 0.003 甲胎蛋白/(ng·mL-1) 61.4±31.2 64.5±29.7 3.015 0.072 总胆红素/(μmol·L-1) 39.7±21.3 48.5±25.8 7.257 0.009 AST/(U·L-1) 55.1±31.2 53.4±30.8 1.016 0.195 ALT/(U·L-1) 56.4±29.4 55.6±33.5 1.157 0.172 白蛋白/(g·L-1) 28.4±8.5 27.6±8.7 1.239 0.148 Child-Pugh评分/分 7.1±2.2 9.7±2.3 5.122 0.019 MELD评分/分 13.2±7.6 17.8±8.1 5.742 0.017 表 2 肝硬化失代偿患者血清SF水平与肝肾功能和甲胎蛋白的相关性分析
统计值 肌酐 甲胎蛋白 总胆红素 AST ALT 白蛋白 Child-Pugh评分 MELD评分 r 0.623 0.367 0.673 -0.239 -0.334 -0.189 0.694 0.712 P 0.012 0.146 0.009 0.227 0.248 0.263 <0.001 <0.001 表 3 影响肝硬化失代偿患者生存情况的Cox单因素和多因素分析
自变量 单因素分析 多因素分析 HR 95%CI P HR 95%CI P 消化道出血 5.237 4.782~5.567 <0.001 4.872 4.256~5.443 0.006 肝性脑病 7.246 6.514~7.882 <0.001 5.134 4.678~5.624 0.005 肌酐 5.123 4.772~5.514 0.008 4.534 4.127~5.103 0.019 总胆红素 4.789 4.213~5.347 0.017 1.125 1.002~1.238 0.086 SF 2.234 1.813~2.653 0.013 1.678 1.213~1.994 0.037 Child-Pugh评分 6.267 5.715~6.625 0.005 4.892 4.335~5.217 0.011 MELD评分 10.247 9.457~10.587 0.002 7.554 7.124~7.996 <0.001 -
[1] 丁惠国, 徐小元, 令狐恩强, 等. 《肝硬化门静脉高压食管胃静脉曲张出血的防治指南》解读[J]. 临床肝胆病杂志, 2016, 32(2): 220-222. doi: 10.3969/j.issn.1001-5256.2016.02.003
[2] 古川, 宋美怡, 孙文静, 等. 2016年肝硬化领域基础与临床研究进展[J]. 中华肝脏病杂志, 2017, 25(1): 5-8. doi: 10.3760/cma.j.issn.1007-3418.2017.01.003
[3] Crismale JF, Friedman SL. Acute Liver Injury and Decompensated Cirrhosis[J]. Med Clin North Am, 2020, 104(4): 647-662. doi: 10.1016/j.mcna.2020.02.010
[4] Trebicka J, Bork P, Krag A, et al. Utilizing the gut microbiome in decompensated cirrhosis and acute-on-chronic liver failure[J]. Nat Rev Gastroenterol Hepatol, 2021, 18(3): 167-180. doi: 10.1038/s41575-020-00376-3
[5] 时克, 张群, 黄云义, 等. 抗肝纤维化治疗对乙型肝炎肝硬化患者发生肝癌的影响[J]. 中华肝脏病杂志, 2021, 29(7): 685-689. doi: 10.3760/cma.j.cn501113-20200227-00072
[6] 翟浩亮, 闻瑜, 朱健, 等. 血清铁蛋白对肝硬化失代偿患者早期死亡的预测价值[J]. 中国卫生检验杂志, 2015, 25(16): 2724-2727. https://www.cnki.com.cn/Article/CJFDTOTAL-ZWJZ201516028.htm
[7] Afify SM, Tabll A, Nawara HM, et al. Five Fibrosis Biomarkers Together with Serum Ferritin Level to Diagnose Liver Fibrosis and Cirrhosis[J]. Clin Lab, 2018, 64(10): 1685-1693.
[8] Mörwald K, Aigner E, Bergsten P, et al. Serum Ferritin Correlates With Liver Fat in Male Adolescents With Obesity[J]. Front Endocrinol(Lausanne), 2020, 11(3): 340.
[9] 程丹, 邵志林, 吴亮, 等. 乙型肝炎肝硬化和肝癌患者血清铁蛋白检测的意义[J]. 实用肝脏病杂志, 2016, 19(6): 736-737. doi: 10.3969/j.issn.1672-5069.2016.06.029
[10] Jung JY, Shim JJ, Park SK, et al. Serum ferritin level is associated with liver steatosis and fibrosis in Korean general population[J]. Hepatol Int, 2019, 13(2): 222-233. doi: 10.1007/s12072-018-9892-8
[11] Sungkar T, Rozi MF, Dairi LB, et al. Serum Ferritin Levels: A Potential Biomarker to Represent Child-Turcotte-Pugh Score among Decompensated Liver Cirrhosis Patients[J]. Malays J Med Sci, 2019, 26(2): 59-65.
[12] 李坤, 沈天白, 李莹. 慢性乙型肝炎和乙型肝炎肝硬化患者血清铁蛋白的变化[J]. 实用肝脏病杂志, 2015, 14(6): 620-623. https://www.cnki.com.cn/Article/CJFDTOTAL-GBSY201506014.htm
[13] Batsaikhan B, Gantumur G, Huang CI, et al. Elevated serum ferritin level associated with hepatic steatosis and fibrosis in hepatitis C virus-infected patients[J]. J Chin Med Assoc, 2019, 82(2): 99-104. doi: 10.1097/JCMA.0000000000000009
[14] Oikonomou T, Goulis I, Soulaidopoulos S, et al. High serum ferritin is associated with worse outcome of patients with decompensated cirrhosis[J]. Ann Gastroenterol, 2017, 30(2): 217-224.
[15] Haghgoo SM, Sharafi H, Alavian SM. Serum cytokines, adipokines and ferritin for non-invasive assessment of liver fibrosis in chronic liver disease: a systematic review[J]. Clin Chem Lab Med, 2019, 57(5): 577-610. doi: 10.1515/cclm-2018-0357
[16] Umer N, Makki MU, Kiran SK, et al. Serum ferritin as a predictor of 30 days mortality in Patients of decompensated chronic liver disease[J]. J Ayub Med Coll Abbottabad, 2017, 29(3): 415-418.
-



 下载:
下载: