A prediction model was constructed to predict the risk of MACE in STEMI patients received PPCI at one year after surgery
-
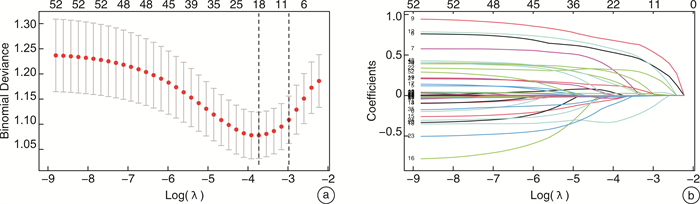
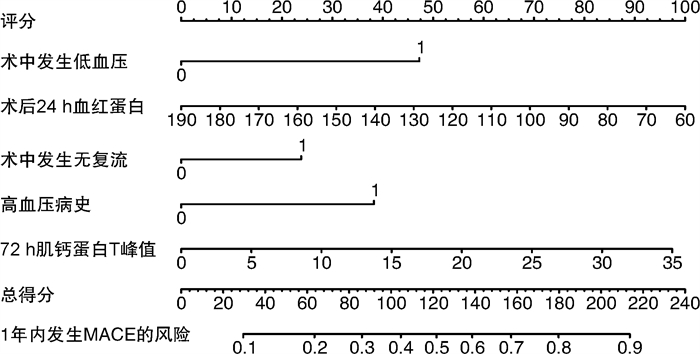
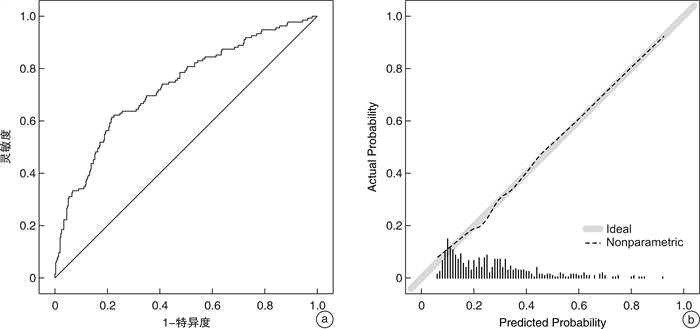
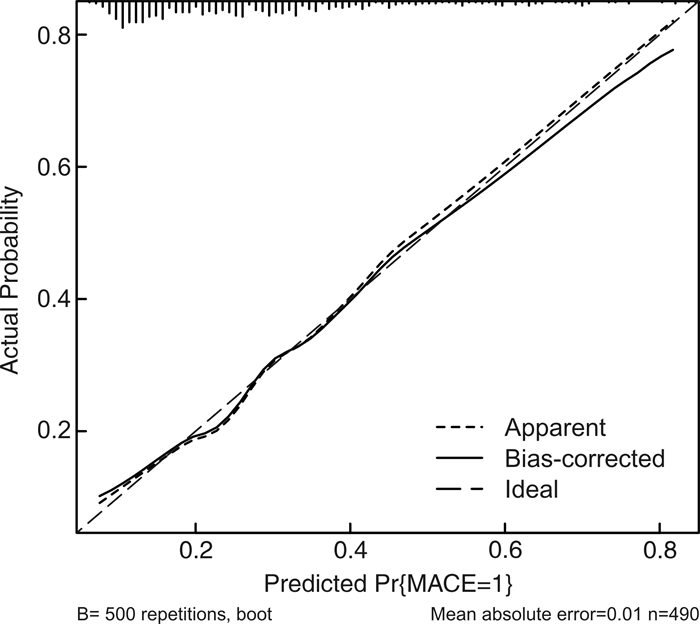
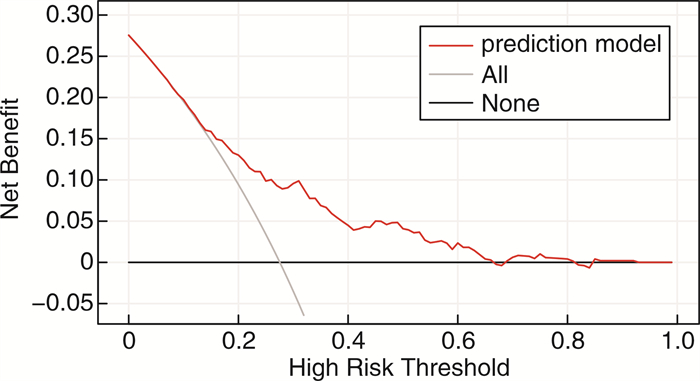
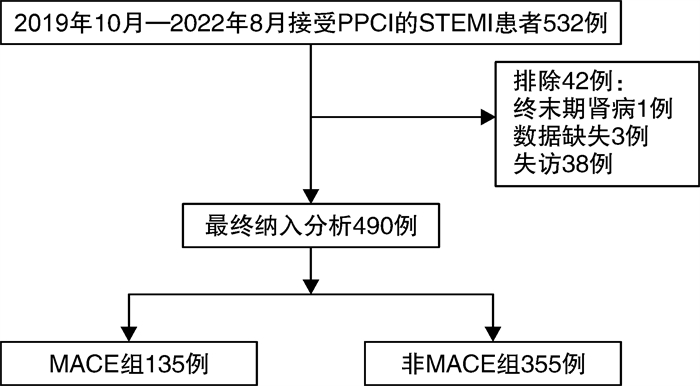
摘要: 目的 建立与验证一个可预测接受直接经皮冠状动脉介入治疗(PPCI)的急性ST段抬高型心肌梗死(STEMI)患者术后1年内发生主要不良心血管事件(MACE)风险的列线图预测模型。方法 本研究是一项回顾性队列研究,选取2019年10月—2022年8月来自新疆自治区人民医院490例行PPCI的STEMI患者为研究对象。应用LASSO回归和logistic多因素回归分析接受PPCI的STEMI患者1年内发生MACE风险的独立危险因素。构建接受PPCI的STEMI患者1年内发生MACE的列线图预测模型,采用ROC曲线、校准曲线进行模型表现评估。并用Bootstrap法进行内部验证,绘制校准曲线、计算C统计量评估模型内部验证表现,绘制DCA临床决策曲线评价模型临床净收益。结果 LASSO回归与多因素logistic回归分析结果显示,入院72 h内肌钙蛋白T峰值升高、术后24 h内血红蛋白水平降低、术中发生低血压、术中发生无复流、既往有高血压病史是接受PPCI的STEMI患者1年内发生MACE的危险因素。模型在本研究人群中的AUC值为0.730(95%CI:0.679~0.782),Hosmer-Lemeshow检验结果提示该模型在本研究人群中有较好的预测准确性。使用Bootstrap法重抽样500次进行内部验证,模型的C指数为0.719,且模型内部验证的校准曲线和理想模型接近,表明模型在内部验证中的区分度及预测准确性较好。DCA临床决策曲线显示该模型在阈值概率范围为0.14~0.66时能够带来临床净获益。结论 本研究构建的简单易用的列线图预测模型可以有效地预测接受PPCI的STEMI患者术后1年内发生MACE的个体化风险。
-
关键词:
- 急性ST段抬高型心肌梗死 /
- 直接经皮冠状动脉介入治疗 /
- 预测模型 /
- 主要不良心血管事件
Abstract: Objective To establish and validate a nomogram prediction model that can predict the risk of major adverse cardiovascular events within 1 year after primary percutaneous coronary intervention in patients with acute ST-segment elevation myocardial infarction.Methods This study is a retrospective cohort study. The 490 patients with STEMI who underwent PPCI from the People's Hospital of Xinjiang Autonomous Region from October 2019 to August 2022 were selected as the research objects. LASSO and logistic regression analysis of independent risk factors for MACE in patients with STEMI undergoing PPCI within 1 year. A nomogram prediction model of MACE within 1 year in STEMI patients undergoing PPCI was constructed, and the model performance was evaluated using ROC curve and calibration curve. Bootstrap method was used for internal verification. The calibration curve was drawn, the C statistic was calculated to evaluate the model's internal validation performance, and the DCA clinical decision curve was drawn to evaluate the model's clinical net benefit.Results LASSO regression and multivariate logistic regression analysis showed that the increase of peak troponin T within 72 hours of admission, the decrease of hemoglobin level within 24 hours after surgery, intraoperative hypotension, intraoperative no reflow, and previous history of hypertension were risk factors for MACE within 1 year in STEMI patients receiving PPCI. The AUC value of the model in the study population was 0.730(95%CI: 0.679-0.782), and the Hosmer-Lemeshow test results suggested that the model had good prediction accuracy in the study population. The Bootstrap method was used to re-sample 500 times for internal verification. The C-index of the model was 0.719, and the calibration curve of the internal verification of the model was close to the ideal model, indicating that the model had good differentiation and prediction accuracy in the internal verification. The DCA clinical decision curve showed that the model could provide a net clinical benefit at a threshold probability range of 0.14-0.66.Conclusion The simple and easy-to-use nomogram prediction model constructed in this study can effectively predict the individualized risk of MACE in STEMI patients receiving PPCI at 1 year after surgery. -

-
表 1 两组临床数据比较
Table 1. Comparison of clinical data
例(%), M(P25, P75), X±S 项目 非MACE组(355例) MACE组(135例) P 男性 303(85.35) 102(75.56) 0.011 年龄 < 60岁 225(63.38) 61(45.19) < 0.001 汉族 200(56.34) 79(58.52) 0.663 本次入院 心率/(次/min) 81.47±14.32 82.61±20.45 0.553 入院时收缩压/mmHg 134.34±22.56 131.20±24.22 0.178 入院时舒张压/mmHg 82.11±15.07 78.47±15.10 0.018 S2D/min 190.00(88.00,330.00) 164.00(88.50,293.00) 0.312 D2W/min 65.00(53.00,86.00) 73.00(59.00,89.50) 0.011 肌红蛋白/(g/L) 78.80(23.00,360.50) 116.00(37.95,447.00) 0.020 肌酸激酶/(U/L) 1 281.00(489.76,2 729.50) 1 440.00(378.50,3 368.00) 0.216 AST/ALT 1.19(0.86,2.50) 1.35(1.00,3.11) 0.028 尿素氮/(mmol/L) 5.40(4.37,6.61) 5.62(4.70,7.11) 0.019 C反应蛋白/(mg/L) 2.62(1.25,5.30) 3.23(1.65,8.51) 0.019 D-二聚体/(ng/mL) 0.30(0.22,0.67) 0.47(0.27,1.08) < 0.001 肌酐/(μmol/L) 68.10(59.70,79.30) 71.80(59.05,88.30) 0.038 乳酸脱氢酶/(U/L) 404.00(237.71,625.52) 496.72(299.21,921.90) 0.001 体质指数 0.016 < 24 kg/m2 95(26.76) 54(40.00) ≥24 kg/m2且 < 28 kg/m2 162(45.63) 48(35.56) ≥28 kg/m2 98(27.61) 33(24.44) 心功能KillipⅠ/Ⅱ级 334(94.08) 108(80.00) < 0.001 既往史 高血压 137(38.59) 82(60.74) < 0.001 高脂血症 130(36.62) 41(30.37) 0.195 糖尿病 80(22.54) 42(31.11) 0.050 吸烟史 180(50.70) 50(37.04) 0.007 心房颤动病史 11(3.10) 5(3.70) 0.958 PCI或CABG史 34(9.58) 15(11.11) 0.613 术中情况 多支病变 167(47.04) 84(62.22) 0.003 行血栓抽吸 30(8.45) 16(11.85) 0.249 IABP 68(19.15) 54(40.00) < 0.001 恶性心律失常 11(3.10) 14(10.37) 0.001 低血压 40(11.27) 42(31.11) < 0.001 心源性休克 8(2.25) 20(14.81) < 0.001 无复流 46(12.96) 33(24.44) 0.002 血管内超声 53(14.93) 24(17.78) 0.439 植入支架个数 0.001 0 25(7.04) 16(11.85) 1个 220(61.97) 57(42.22) 2个 94(26.48) 53(39.26) ≥3个 16(4.51) 9(6.67) 院内情况 胆固醇/(mmol/L) 4.95±1.13 4.65±1.12 0.009 高密度脂蛋白/(mmol/L) 1.12±0.33 1.12±0.25 0.956 低密度脂蛋白/(mmol/L) 3.15±0.96 2.88±0.88 0.004 术后24 h内血红蛋白/(ng/L) 147.83±16.27 140.67±21.12 < 0.001 总胆红素/(μmol/L) 13.24(9.56,18.30) 13.80(10.11,17.65) 0.597 尿酸峰值/(μmol/L) 375.00(311.28,449.45) 395.00(318.61,481.10) 0.152 肌酸激酶同工酶峰值/(ng/mL) 159.50(70.70,300.00) 172.00(97.10,300.00) 0.303 肌钙蛋白T峰值/(ng/L) 2.78(0.71,5.65) 4.42(1.93,8.79) < 0.001 肌钙蛋白I峰值/(ng/L) 30.96(3.75,50.00) 41.40(9.35,50.00) 0.126 最低左心室射血分数/% 50.60±5.98 48.11±7.31 < 0.001 降钙素原/(ng/mL) 0.05(0.03,0.07) 0.06(0.04,0.13) < 0.001 复合指标 TyG 9.05±0.68 9.21±0.71 0.018 NLR 11.32(7.39,16.70) 12.49(7.76,19.40) 0.112 PLR 251.47(174.88,344.83) 246.55(153.54,373.79) 0.905 MLR 0.48(0.29,0.74) 0.52(0.31,0.87) 0.219 WMR 1.00(0.80,1.24) 1.03(0.80,1.35) 0.439 表 2 多因素logistic回归分析结果
Table 2. Multivariate logistic regression analysis results
变量 Beta Z P OR(95%CI) 入院72 h内肌钙蛋白T峰值 0.05 2.05 0.040 1.05(1.01~1.10) 术后24 h内血红蛋白 -0.02 -2.77 0.006 0.98(0.97~0.99) 院内最低左室射血分数 -0.03 -1.68 0.093 0.97(0.94~1.01) 术中发生心源性休克 1.01 1.91 0.056 2.73(0.97~7.68) 术中发生低血压 0.72 2.25 0.024 2.06(1.10~3.86) 术中发生无复流 0.60 2.13 0.033 1.83(1.05~3.17) 既往有高血压病史 0.88 3.89 < 0.001 2.41(1.55~3.76) 心功能Killip Ⅲ/Ⅳ级 0.58 1.57 0.117 1.79(0.87~3.68) -
[1] 中华医学会心血管病学分会. 急性ST段抬高型心肌梗死诊断和治疗指南(2019)[J]. 中华心血管病杂志, 2019(10): 766-767.
[2] Yellon DM, Hausenloy DJ. Myocardial reperfusion injury[J]. N Engl J Med, 2007, 357(11): 1121-1135. doi: 10.1056/NEJMra071667
[3] Frohlich GM, Meier P, White SK, et al. Myocardial reperfusion injury: looking beyond primary PCI[J]. Eur Heart J, 2013, 34(23): 1714-1722. doi: 10.1093/eurheartj/eht090
[4] Frangogiannis NG. The immune system and cardiac repair[J]. Pharmacol Res, 2008, 58(2): 88-111. doi: 10.1016/j.phrs.2008.06.007
[5] Frangogiannis NG. Regulation of the inflammatory response in cardiac repair[J]. Circ Res, 2012, 110(1): 159-173. doi: 10.1161/CIRCRESAHA.111.243162
[6] Fox KA, Dabbous OH, Goldberg RJ, et al. Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: prospective multinational observational study(GRACE)[J]. BMJ, 2006, 333(7578): 1091. doi: 10.1136/bmj.38985.646481.55
[7] Morrow DA, Antman EM, Charlesworth A, et al. TIMI risk score for ST-elevation myocardial infarction: A convenient, bedside, clinical score for risk assessment at presentation: An intravenous nPA for treatment of infarcting myocardium early Ⅱ trial substudy[J]. Circulation, 2000, 102(17): 2031-2037. doi: 10.1161/01.CIR.102.17.2031
[8] Kaur G, Baghdasaryan P, Natarajan B, et al. Pathophysiology, diagnosis, and management of coronary no-reflow phenomenon[J]. Int J Angiol, 2022, 31(2): 107-112. doi: 10.1055/s-0041-1735949
[9] Liu Y, Ye T, Chen K, et al. A nomogram risk prediction model for no-reflow after primary percutaneous coronary intervention based on rapidly accessible patient data among patients with ST-segment elevation myocardial infarction and its relationship with prognosis[J]. Front Cardiovasc Med, 2022, 9: 966299. doi: 10.3389/fcvm.2022.966299
[10] Ye Z, Xu Y, Tang L, et al. Predicting long-term prognosis after percutaneous coronary intervention in patients with new onset ST-elevation myocardial infarction: development and external validation of a nomogram model[J]. Cardiovasc Diabetol, 2023, 22(1): 87. doi: 10.1186/s12933-023-01820-9
[11] 张子龙, 沈鑫, 何林龙, 等. 构建预测模型预测老年STEMI患者PCI术后3年内主要不良心血管事件的发生风险[J]. 海南医学院学报, 2021, 27(11): 827-833.
[12] 翟虎, 张纯溪, 王禹, 等. 急性ST段抬高型心肌梗死患者急诊介入前心室颤动预测模型构建及验证[J]. 临床心血管病杂志, 2023, 39(6): 459-465. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2023.06.010
[13] Soeiro AM, Silva P, Roque E, et al. Prognostic differences between men and women with acute coronary syndrome. data from a brazilian registry[J]. Arq Bras Cardiol, 2018, 111(5): 648-653.
[14] Pedrinelli R, Ballo P, Fiorentini C, et al. Hypertension and acute myocardial infarction: an overview[J]. J Cardiovasc Med(Hagerstown), 2012, 13(3): 194-202. doi: 10.2459/JCM.0b013e3283511ee2
[15] Chandrashekhar Y, Alexander T, Mullasari A, et al. Resource and infrastructure-appropriate management of ST-segment elevation myocardial infarction in low-and middle-income countries[J]. Circulation, 2020, 141(24): 2004-2025. doi: 10.1161/CIRCULATIONAHA.119.041297
[16] Montone RA, Camilli M, Del BM, et al. No-reflow: update on diagnosis, pathophysiology and therapeutic strategies[J]. G Ital Cardiol(Rome), 2020, 21(6 Suppl 1): 4S-14S.
[17] 顾冬冬, 程键, 孔菲菲, 等. 血清Galectin-9、CXCL10对急性心肌梗死患者急诊PCI术后慢血流现象的预测效能[J]. 分子诊断与治疗杂志, 2023, 15(9): 1515-1519. doi: 10.3969/j.issn.1674-6929.2023.09.012
[18] Papapostolou S, Andrianopoulos N, Duffy SJ, et al. Long-term clinical outcomes of transient and persistent no-reflow following percutaneous coronary intervention(PCI): a multicentre Australian registry[J]. Euro Intervention, 2018, 14(2): 185-193.
[19] Dutsch A, Graesser C, Voll F, et al. Association of in-hospital hemoglobin drop with decreased myocardial salvage and increased long-term mortality in patients with acute ST-segment-elevation myocardial infarction[J]. J Am Heart Assoc, 2022, 11(17): e24857.
[20] Leonardi S, Gragnano F, Carrara G, et al. Prognostic implications of declining hemoglobin content in patients hospitalized with acute coronary syndromes[J]. J Am Coll Cardiol, 2021, 77(4): 375-388. doi: 10.1016/j.jacc.2020.11.046
[21] Zeren G, Avci II, Simsek B, et al. Post percutaneous coronary intervention hemoglobin levels predict in-hospital mortality in patients with STEMI treated with primary percutaneous coronary intervention[J]. Anatol J Cardiol, 2021, 25(9): 623-629. doi: 10.5152/AnatolJCardiol.2021.07282
[22] Giannitsis E, Muller-Bardorff M, Lehrke S, et al. Admission troponin T level predicts clinical outcomes, TIMI flow, and myocardial tissue perfusion after primary percutaneous intervention for acute ST-segment elevation myocardial infarction[J]. Circulation, 2001, 104(6): 630-635. doi: 10.1161/hc3101.093863
[23] Chia S, Senatore F, Raffel OC, et al. Utility of cardiac biomarkers in predicting infarct size, left ventricular function, and clinical outcome after primary percutaneous coronary intervention for ST-segment elevation myocardial infarction[J]. JACC Cardiovasc Interv, 2008, 1(4): 415-423. doi: 10.1016/j.jcin.2008.04.010
[24] Tzivoni D, Koukoui D, Guetta V, et al. Comparison of Troponin T to creatine kinase and to radionuclide cardiac imaging infarct size in patients with ST-elevation myocardial infarction undergoing primary angioplasty[J]. Am J Cardiol, 2008, 101(6): 753-757. doi: 10.1016/j.amjcard.2007.09.119
[25] Efron B. Estimation and Accuracy after Model Selection[J]. J Am Stat Assoc, 2014, 109(507): 991-1007. doi: 10.1080/01621459.2013.823775
-



 下载:
下载: