Correlation study of TyG index and recurrence of atrial fibrillation within 1 year after radiofrequency ablation in non-diabetic patients
-
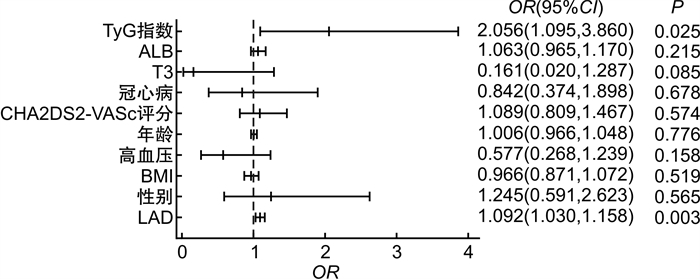
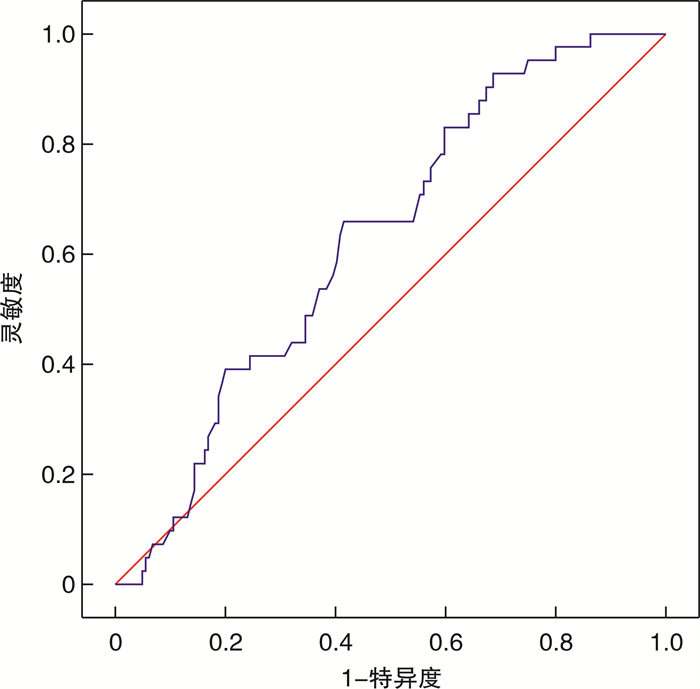
摘要: 目的 探讨甘油三酯葡萄糖(TyG)指数与射频消融术后心房颤动(房颤)1年内复发之间的关联。方法 回顾性选取200例首次行射频消融术的房颤患者,收集患者的临床资料和术后12个月的随访数据,观察患者是否出现房颤复发,依据随访结果将患者分为复发组和未复发组。比较两组TyG指数的差异,分析影响房颤复发的危险因素及独立预测因子。结果 相较于非复发组,房颤复发组患者的TyG指数明显升高(8.70±0.06 vs 8.48±0.04,P < 0.05)。多因素回归分析显示,TyG指数是射频消融术后房颤复发的独立危险因素。受试者工作特征曲线示房颤复发TyG指数曲线下面积为0.627(95%CI0.541~0.714,P < 0.05),预测房颤复发的截断值为8.59。结论 术前高水平TyG指数提示房颤患者射频消融术后具有较高的复发风险。Abstract: Objective This study investigated the association between triglyceride glucose(TyG) index and the recurrence of atrial fibrillation(AF) within 1 year after radiofrequency ablation.Methods The 200 patients with AF who underwent radiofrequency ablation for the first time were retrospectively selected. Clinical data and follow-up data after surgery 12 months were collected. According to the follow-up results, patients were divided into recurrence group and non-recurrence group. The difference of TyG index between the two groups was compared.Results Compared with the non-recurrent group, the TyG index in the recurrent group was significantly increased(8.70±0.06 vs 8.48±0.04, P < 0.05). Multivariate regression analysis showed that TyG index was an independent risk factor for recurrent AF after radiofrequency ablation. The area under curve of TyG index was 0.627(95%CI 0.541-0.714, P < 0.05), and the best cut-off value of TyG index in predicting AF recurrence was 8.59.Conclusion High TyG index indicates that patients with AF have a higher risk of recurrence after radiofrequency ablation.
-
Key words:
- atrial fibrillation /
- radiofrequency ablation /
- triglyceride glucose index /
- recurrence
-

-
表 1 两组基线资料比较
Table 1. General data
例(%), X±S, M(P25, P75) 项目 复发组(41例) 未复发组(159例) t/Z/χ2 P 男性 26(63.4) 105(66.0) 0.099 0.753 年龄/岁 60.68±1.7 61.03±0.74 0.206 0.837 BMI/(kg/m2) 26.20±0.55 25.86±0.25 0.610 0.545 高血压病 22(53.7) 89(56.0) 0.071 0.790 冠心病 9(22.0) 39(24.5) 0.119 0.730 饮酒史 9(22.0) 39(24.5) 0.119 0.730 吸烟史 12(29.2) 56(35.2) 0.515 0.473 房颤类型 阵发性 21(51.2) 83(52.2) 0.013 0.911 持续性 20(48.8) 76(47.8) CHA2DS2-VASc评分/分 2(1,3) 2(1,3) -0.545 0.586 表 2 两组实验室指标比较
Table 2. Comparison of laboratory indicators
X±S, M(P25, P75) 项目 复发组(41例) 未复发组(159例) t/Z P WBC/(×109/L) 5.84±0.18 5.87(4.94,6.94) -0.209 0.835 NEUT/(×109/L) 3.19±0.13 3.12(2.52,3.94) -0.159 0.874 LYM/(×109/L) 2.00±0.09 2.04(1.57,2.43) -0.079 0.937 NLR 1.61(1.27,2.06) 1.57(1.22,2.06) -0.490 0.624 MXD/(×109/L) 0.46±0.02 0.46(0.37,0.56) -0.245 0.806 EOS/(×109/L) 0.11(0.05,0.15) 0.11(0.06,0.18) -0.091 0.928 BASO/(×109/L) 0.03(0.02,0.05) 0.03(0.02,0.05) -1.039 0.299 HGB/(g/L) 150(137,160) 148.49±1.34 -0.045 0.964 PLT/(×109/L) 196(169,235) 202(169,231) -0.169 0.865 UREA/(mmol/L) 5.43(5.01,6.79) 5.61(4.75,6.76) -0.012 0.905 FBG/(mmol/L) 5.17±0.11 4.93(4.52,5.28) -1.658 0.097 UA/(μmol/L) 358(310,428) 339(288,418) -0.944 0.345 TP/(g/L) 68.37±0.79 67.17±0.47 -1.339 0.181 ALB/(g/L) 40.91±0.55 40.00±0.28 -1.300 0.194 GLB/(g/L) 27.47±0.53 26.78±0.38 -0.758 0.448 A/G 1.515±0.04 1.500(1.30,1.66) -0.312 0.755 TG/(mmol/L) 1.48(1.13,2.06) 1.21(0.88,1.74) -2.323 0.020 TC/(mmol/L) 4.07±0.18 3.77(3.13,4.40) -1.164 0.245 LDL-C/(mmol/L) 2.46±0.14 2.21(1.61,2.69) -1.628 0.103 TSH/(μIU/mL) 2.08(1.49,4.34) 2.08(1.33,3.22) -1.048 0.295 T3/(ng/mL) 1.06±0.02 1.10±0.01 1.375 0.171 T4/(μg/dL) 7.4(6.5,7.9) 7.4(6.5,8.3) -0.708 0.479 糖化血红蛋白/% 5.65±0.55 5.70(5.50,5.90) -1.336 0.181 D-D/(μg/mL) 0.16(0.11,0.25) 0.18(0.12,0.27) -1.166 0.244 TyG指数 8.70±0.06 8.48±0.04 2.933 0.004 表 3 两组患者超声影像学指标对比
Table 3. Ultrasonic imaging index
X±S, M(P25, P75) 指标 复发组(41例) 未复发组(159例) t/Z P 右房上下径/mm 51.93±1.12 50(45,56) -0.730 0.465 右房左右径/mm 44.46±1.06 42(38,49) -0.836 0.403 主肺动脉内径/mm 24.78±0.38 25(23,26) -0.061 0.951 LVEED/mm 49.27±0.61 49(47,52) -0.434 0.664 LAD/mm 43.95±0.86 41.66±0.48 2.215 0.028 LVEF/% 64.73(62.02,67.42) 65.81(61.90,68.97) -1.102 0.271 表 4 TG与TyG指数共线性统计
Table 4. Collinearity statistics of TG and TyG index
项目 容差 VIF TG 0.188 5.311 TyG指数 0.187 5.356 -
[1] 黄青云, 李文彦, 杨曼, 等. 射频消融联合左心耳封堵治疗非瓣膜性心房颤动的长期有效性及安全性研究[J]. 临床心血管病杂志, 2023, 39(7): 541-546. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2023.07.010
[2] Hindricks G. Corrigendum to: 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery(EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology(ESC)Developed with the special contribution of the European Heart Rhythm Association(EHRA)of the ESC[J]. Eur Heart J, 2021, 42(40): 4194. doi: 10.1093/eurheartj/ehab648
[3] Poole JE. Recurrence of atrial fibrillation after catheter ablation or antiarrhythmic drug therapy in the CABANA Trial[J]. J Am Coll Cardiol, 2020, 75(25): 3105-3118. doi: 10.1016/j.jacc.2020.04.065
[4] Erhard N, Metzner A, Fink T. Late arrhythmia recurrence after atrial fibrillation ablation: incidence, mechanisms and clinical implications[J]. Herzschrittmacherther Elektrophysiol, 2022.33(1): 71-76. doi: 10.1007/s00399-021-00836-6
[5] Tao LC. Triglyceride-glucose index as a marker in cardiovascular diseases: landscape and limitations[J]. Cardiovasc Diabetol, 2022, 21(1): 68. doi: 10.1186/s12933-022-01511-x
[6] Chen S. Association between triglyceride-glucose index and atrial fibrillation: A retrospective observational study[J]. Front Endocrinol(Lausanne), 2022, 13: 1047927. doi: 10.3389/fendo.2022.1047927
[7] Tang Q. The pre-ablation triglyceride-glucose index predicts late recurrence of atrial fibrillation after radiofrequency ablation in non-diabetic adults[J]. BMC Cardiovasc Disord, 2022, 22(1): 219. doi: 10.1186/s12872-022-02657-y
[8] Kosmas CE. Insulin resistance and cardiovascular disease[J]. J Int Med Res, 2023, 51(3): 3000605231164548. doi: 10.1177/03000605231164548
[9] DeFronzo RA. Insulin resistance, lipotoxicity, type 2 diabetes and atherosclerosis: the missing links. The Claude Bernard Lecture 2009[J]. Diabetologia, 2010, 53(7): 1270-1287. doi: 10.1007/s00125-010-1684-1
[10] Yaribeygi H. Insulin resistance: Review of the underlying molecular mechanisms[J]. J Cell Physiol, 2019, 234(6): 8152-8161. doi: 10.1002/jcp.27603
[11] Staerk L. Atrial fibrillation: epidemiology, pathophysiology, and clinical outcomes[J]. Circ Res, 2017, 120(9): 1501-1517. doi: 10.1161/CIRCRESAHA.117.309732
[12] O'Keefe EL. Prevention and treatment of atrial fibrillation via risk factor modification[J]. Am J Cardiol, 2021, 160: 46-52. doi: 10.1016/j.amjcard.2021.08.042
[13] Chan YH. Atrial fibrillation and its arrhythmogenesis associated with insulin resistance[J]. Cardiovasc Diabetol, 2019, 18(1): 125. doi: 10.1186/s12933-019-0928-8
[14] Wang Z. Effect of insulin resistance on recurrence after radiofrequency catheter ablation in patients with atrial fibrillation[J]. Cardiovasc Drugs Ther, 2023, 37(4): 705-713. doi: 10.1007/s10557-022-07317-z
[15] Buist TJ, Zipes DP, Elvan A. Atrial fibrillation ablation strategies and technologies: past, present, and future[J]. Clin Res Cardiol, 2021, 110(6): 775-788. doi: 10.1007/s00392-020-01751-5
[16] Zhang Y. Intermittent fasting attenuates obesity-related atrial fibrillation via SIRT3-mediated insulin resistance mitigation[J]. Biochim Biophys Acta Mol Basis Dis, 2023, 1869(4): 166638. doi: 10.1016/j.bbadis.2023.166638
[17] Ling Y, Fu C, Fan Q, et al. Triglyceride-glucose index and new-onset atrial fibrillation in ST-segment elevation myocardial infarction patients after percutaneous coronary intervention[J]. Front Cardiovasc Med, 2022, 9: 838761. doi: 10.3389/fcvm.2022.838761
[18] Barzegar N, Tohidi M, Hasheminia M, et al. The impact of triglyceride-glucose index on incident cardiovascular events during 16 years of follow-up: Tehran Lipid and Glucose Study[J]. Cardiovasc Diabetol, 2020, 19(1): 155. doi: 10.1186/s12933-020-01121-5
[19] 孙梓宜, 王子涵, 陈颖, 等. TyG指数联合血管功能指标对冠状动脉狭窄程度的预测价值[J]. 临床心血管病杂志, 2022, 38(1): 17-21. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2022.01.004
[20] Duran EK. Triglyceride-rich lipoprotein cholesterol, small dense LDL cholesterol, and incident cardiovascular disease[J]. J Am Coll Cardiol, 2020.75(17): 2122-2135. doi: 10.1016/j.jacc.2020.02.059
[21] Samuel VT, Shulman GI. The pathogenesis of insulin resistance: integrating signaling pathways and substrate flux[J]. J Clin Invest, 2016, 126(1): 12-22. doi: 10.1172/JCI77812
[22] Zakynthinos GE, Tsolaki V, Oikonomou E, et al. Metabolic syndrome and atrial fibrillation: different entities or combined disorders[J]. J Pers Med, 2023, 13(9): 110.
[23] Scridon A, Dobreanu D, Chevalier P, et al. Inflammation, a link between obesity and atrial fibrillation[J]. Inflamm Res, 2015, 64(6): 383-393. doi: 10.1007/s00011-015-0827-8
[24] Liu X. U-shaped association between the triglyceride-glucose index and atrial fibrillation incidence in a general population without known cardiovascular disease[J]. Cardiovasc Diabetol, 2023, 22(1): 118. doi: 10.1186/s12933-023-01777-9
[25] 张宁, 叶宝兰, 程雪妮. 射频消融术后心房颤动复发的影响因素分析[J]. 临床医学研究与实践, 2022, 7(34): 41-43.
-




 下载:
下载: